On average, 10% of teens each year struggle with depression. Yet the majority of parents miss the early warning signs.
Depression also afflicts younger children, although less frequently.
Adolescent peer pressure, insecurity, conflict with parents, and a pervasive sense of not living up to expectations cause teens to be more vulnerable to depression.
It is a growing problem with grave consequences. In the short term, depressed teens are more likely to experience academic failure, social isolation, substance abuse, and become at higher risk for self-harm and suicide.
Long-term, it can lead to chronic mental health disorders, lower income, and dysfunctional adult relationships.
The good news? It can be treated effectively, and these risks can subsequently be mitigated.
The key is for parents to recognize when their child is not just ‘going through a phase’ but is genuinely depressed.
Depression: What To Look For
You may be wondering what depression looks like in a child or teen. The short answer, it looks pretty much like depression in an adult. This includes:
Acting sad (moping around the house, slouched posture, unhappy facial expression)
Crying frequently
Changes in sleep (this could be increased sleep, decreased sleep, problems getting to sleep, etc.)
Changes in appetite (dramatic increases or reductions in appetite, often with changes in body weight).
Lack of energy (they play less, move less, are harder to get moving into the car, to the dinner table, out of bed in the morning, etc.)
Becoming socially withdrawn and harder to engage (both with friends and family)
Changes in attention/concentration. Your child has gone from having adequate focus to having a difficult time concentrating on homework, or other subjects.
Anhedonia. That is, failing to find pleasure in activities that had been (and normally are) pleasurable. (The youngster who enjoyed sports no longer engages in competition, or the teen who had loved listening to music now seldom does so).
Feeling helpless or hopeless.
You will find those same symptoms in adult depression. The one difference is that children/teens are more inclined than adults to express their depression by acting out and having angry outbursts in addition to the above symptoms.
It’s fair to say when looking over this list of symptoms, “Every child does these things from time to time. How can I tell when these symptoms mean my kiddo is depressed?” Great question.
To figure this out, therapists look at each symptom, how frequently it occurs, how intense it is, how long the symptom has been observed, etc. They then refer to the DSM to judge whether the overall picture, in light of the data gathered, fits the criteria for a depressive disorder.
There is no reason to expect parents to go through that sort of analysis. So, for our purposes, we will simplify things and take the following approach.
ONE If your child has three of the symptoms listed above, and they have lasted for a month or more, consult your pediatrician.
TWO Go to the following website (CLICK HERE) and complete a brief, online, child/teen mental health quiz.
Reviewing your answers to questions and the immediate results from completing the questionnaire will help you organize your thoughts and clarify whether your child’s struggles are outside the norm.
Helping the Depressed Child or Adolescent
If you have a child who is depressed, you need to act decisively.
Take the following approach.
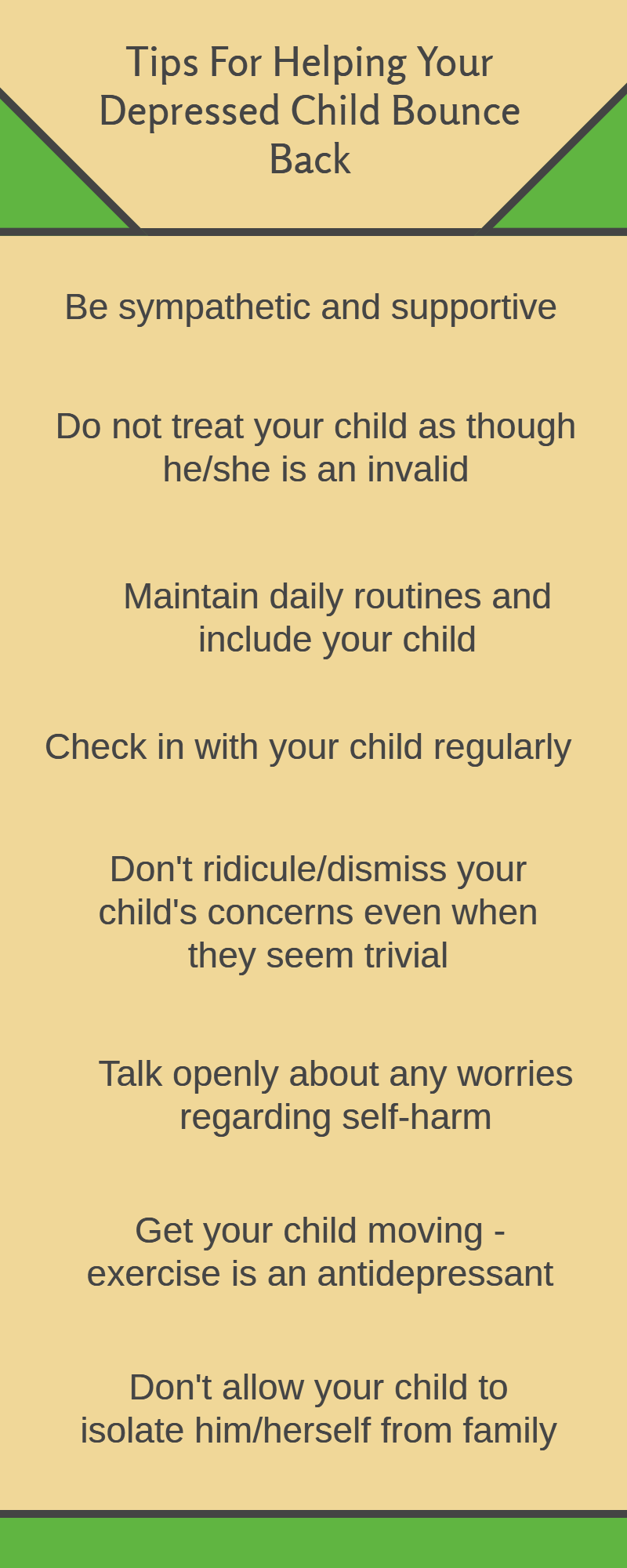
1. Be sympathetic and supportive. Your attitude will do wonders.
2. While being sympathetic and supportive, don’t treat your child like an invalid. He or she still needs to go to school, complete homework, honor obligations, finish chores, etc. In other words, life goes on even when one is depressed. This is a good time for your child to learn to be tough. It is one of the single most important qualities you can build to help your son or daughter push through and succeed in life.
3. Keep up your routines at home. Routines are reassuring for those who are depressed. It provides a sense of stability and predictability.
4. Check in with your child regularly. Let your son, or daughter, know that you are worried. Tell them you know they are struggling; you are there to help or simply to listen. Also, inform your child that you will be checking in with them every evening before bedtime and asking if they would like to talk. They may object, but patiently persist. Reassure them that they won’t have to talk if they don't want to, but you’ll still check in with them.
5. Some of the reasons a child will give for being depressed may appear foolish to adults (and to their teenage siblings, but then again, much of the world seems laughable when you are a teen). I've known parents who gently tease their child about these concerns. They do so in order to provide perspective and 'shake them out of their self-pity.' I won't preach. Let's just agree that it won't be helpful for anyone in the family to make fun of, or be dismissive of, the concerns a depressed youngster expresses.
After showing your child that you take his or her concerns seriously, move on to provide a more realistic view. Children need that perspective
6. If you begin to worry that your child is so depressed that he, or she, is at risk of harming themselves, have a very direct talk about your concerns.
Some of you may have heard that talking about self-harm, and suicide just pushes a child toward that self-destructive behavior. That is not true. Most children who are considering this ‘solution’ find it reassuring to have their parent bring up the topic.
If you have concerns about your child being at risk for attempting suicide consult with a professional. Do so right away.
7. Exercise is helpful.
Numerous studies show that regular vigorous exercise helps alleviate depressive symptoms. Exercise is an all-natural treatment to fight depression - Harvard Health
Get your child/teen out of the house on a walk, bike ride, skateboarding, etc. This should be done daily. Most cities will have plenty of opportunities to help you find enticing ways to get your child active. In my town of Folsom, for example, there are miles of hiking trails, numerous arts and crafts activities , organized sports, and numerous other opportunities to get active.
8. Depressed people (even children) tend to isolate themselves from others. This drastically worsens their depression. Don’t let your child become isolated at home. It can be a struggle. Don’t give in. Sure, your child needs some alone time, but he/she should still be involved with family meals, chore time, running errands, move/game nights, etc.
9. Insist your child socialize with peers. Each boy and girl is different in how they prefer to socialize. There is no one size fits all. The main thing is to not let your child become socially isolated.
10. We’ve covered this earlier – work with your pediatrician on ways to resolve the depression.
More Options For Helping The Depressed Child/Adolescent
If you have tried the above suggestions and your child remains just as depressed two or three weeks later, it is time to look at other options. This might be to seek out counseling. It could be a medication trial (honestly, a last resort, except under exceptional circumstances). You could consider both options being used at the same time.
To wade through these choices, you need information that guides you to the best decision. There are resources you can turn to for helping you select a great therapist and know when to employ medication to assist in solving problems such as depression and anxiety.
Conclusion
Childhood depression is not uncommon, but it doesn't have to become a permanent fixture in your family's life. You now have the clarity needed to recognize when your child has crossed the line from having a bad week to being genuinely depressed. You also have a roadmap for decisive action.
Remember: your depressed child needs your sympathy, but they also need you to refuse to let them become an emotional invalid. No one wants their child to become depressed, but if it happens, consider it an opportunity for your child to build greater resilience and mental toughness.
Your son or daughter needs structure, clear expectations, and the opportunity to learn one of life's most valuable lessons—that they can be tough, push through hard times, and come out stronger on the other side.
That's not just how you help your child overcome depression. It's how you help them build a life that matters.